Nephrology
Renal pathophysiology in Fabry disease
The information on this page is tailored for nephrologists. For more detailed information on the cause, inheritance, diagnosis and management of Fabry disease, please refer to our ‘About Fabry disease’ page.
This short video provides an overview of the renal impact of Fabry disease, including how podocytes are affected by lysosomal substrate accumulation.
Pathology in Fabry disease arises from accumulation of globotriaosylceramide (GL-3) which leads to cellular dysfunction. Specifically, a cascade of events is triggered which includes oxidative stress, compromised metabolism and cell death resulting in vascular dysfunction and tissue fibrosis.1,2
One of the major organ systems which is principally affected in Fabry disease is the renal system. Damage to the kidneys and impairment of renal function contributes greatly towards morbidity and mortality. Severity also increases with age.1
Click on the headings to learn more about the proposed mechanisms of renal pathology.
Older Fabry patients (25–50 years) often display a consistent alteration in which arterial fibroid deposits are found in the kidney. These deposits are caused by necrosis of smooth muscle cells in the arterial wall after they become overloaded by GL-3 accumulation. Vascular damage of this kind leads to ischaemic changes which cause dysfunction and death of several cell types in the kidney.
GL-3 accumulation in podocytes causes irreversible damage which eventually leads to cell death. Extracellular matrix proteins in renal vasculature begin to accumulate at the site of damage, causing glomerulosclerosis and eventual loss of kidney function.
Deposition of GL-3 in these cells may lead to tubular atrophy and eventual loss of function. Other glomeruli may undergo hypertrophy in order to compensate for this loss of function, leading to hyperfiltration and then glomerulosclerosis which contributes to further damage.
Renal progression in Fabry disease
The image below summarises typical renal progression in Fabry disease patients.
Tap on each dot to learn moreAdapted from Germain 2010 and Ortiz et al 2018.1,4
Reproduced with permission from Germain DP et al., 2010.1
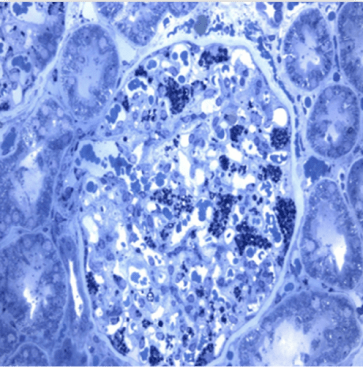
In Fabry disease, renal GL-3 deposition is detectable using light microscopy on biopsy tissue, as shown in this image.
NP-NN-UK-00130325
April 2025
- Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5:30.
- Rombach SM, Twickler TB, Aerts JMFG, et al. Vasculopathy in patients with Fabry disease: current controversies and research directions. Molec Genet Metab. 2010;99:99–108.
- Alroy J, Sabnis S, Kopp JB. Renal pathophysiology in Fabry disease. J Am Soc Nephrol. 2002;13:S134–138.
- Ortiz A, Germain DP, Desnick RJ, et al. Fabry disease revisited: management and treatment recommendations for adult patients. Mol Genet Metab. 2018;123:416–427.