About Fabry disease
GLA gene mutations and inheritance
To date, there are more than 1000 known mutations of the GLA gene that give rise to Fabry disease. In most patients, a single point mutation is enough to cause disease. However, different mutations cause varying symptoms and severity.1
This graphic shows the different types of GLA mutation which may give rise to the classic and late-onset Fabry phenotypes.
Classic phenotype
- Caused by GLA mutations that significantly alter α-Gal A so it has little or no activity2
- Mutations include:3
- Large and small gene rearrangements
- Splicing defects
- Missense or nonsense variants
Late–onset phenotype
- Caused by GLA mutations that reduce the effectiveness of α-Gal A but result in some residual activity2
- Mutations include:3
- Missense variants
- Splicing defects
Examples of known GLA variants
Many of the GLA mutations seen in patients with Fabry disease involve the hydrophobic core of the α-Gal A dimer, not just the active site. This suggests Fabry disease is primarily a condition of abnormal protein folding. This diagram illustrates the location of many of the known mutations. Changes to the active site are coloured red, the core of the enzyme in blue and other changes in yellow. The green ligand indicates the location of the active site.4
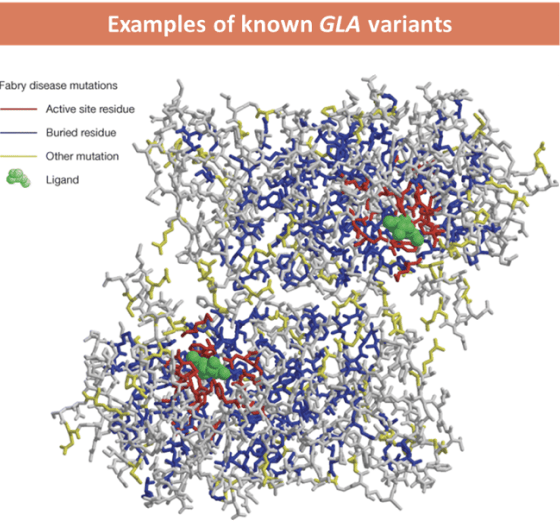
Reproduced with permission from Garman SC. 2007.4
Genotype-phenotype correlation
In many cases, it is difficult to make clear links between genotype and phenotype for several reasons
Most pathogenic GLA variants are specific to a single family, and even individuals within the same family show significant variation in symptoms and severity3
The common signs and symptoms of late-onset Fabry (e.g. stroke or cardiomyopathy) can have many other causes. In patients with a GLA mutation, it can be difficult to determine whether these symptoms have been caused by the mutation or another factor3
Some specific pathogenic GLA variants have been found in both people with the classic and later-onset phenotypes, suggesting there are other factors influencing how the condition affects different individuals3
The GLA gene lies on the X-chromosome, making Fabry disease an X-linked condition. As a result, males are more likely to be severely affected than females, as they only have one X-chromosome and one (mutated) GLA gene.2
Females and Fabry disease
In the past, females were thought to be asymptomatic carriers. It is now known females with Fabry disease can exhibit a range of symptoms and disease severity, from asymptomatic to as severe as male patients.5 The variation in phenotype seen in female patients is thought to be related to X-chromosome inactivation and mosaicism effects.5 Skewed X-chromosome inactivation may result in a higher proportion of the mutant GLA gene being expressed in a particular tissue (e.g. cardiac), producing localised symptoms.5
Family cascade screening
Once Fabry disease has been diagnosed, genetic testing may be offered to family members to assess the risk of developing symptoms and the potential need for treatment. However, fathers of affected sons, and sons of affected fathers, should not have inherited a faulty gene so testing is not needed.3 All female relatives of an affected individual should be offered genetic counselling and testing if requested.3 Finally, at-risk females may wish to consider genetic testing before pregnancy as prenatal testing and pre-implantation genetic diagnosis are possible.3
NP-NN-UKI-00051024
October 2024
- Tuttolomondo A, Simonetta I, Duro G, et al. Inter-familial and intra-familial phenotypic variability in three Sicilian families with Anderson-Fabry disease. Oncotarget. 2017;8:61415–61424.
- National Organization for Rare Disorders (NORD). Fabry Disease. 2019. Available at https://rarediseases.org/rare-diseases/fabry-disease/. Accessed July 2022.
- Mehta A, Hughes DA. Fabry disease. 2002 Aug 5 [Updated 2017 Jan 5]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020.
- Garman SC. Structure-function relationships in α-galactosidase A. Acta Paediatr. 2007;96:6–16.
- Germain DP. Fabry disease. Orphanet J Rare Dis. 2010;5:30.